Patients who undergo hematopoietic cell transplantation (HCT) for consolidation of acute myeloid leukemia (AML) remission remain at risk of relapsing, and early warning or diagnosis of relapse can lead to effective interception approaches. Targeted small-molecule or cellular immunotherapy can be used in prevention or pre-emption.
A plenary session on Saturday, Feb. 7, will explore the latest diagnostic and therapeutic developments aimed at the detection, treatment and prevention of measurable residual disease (MRD) post-transplant. Eradicating Disease and Prevention of Relapse: Novel Agents and Cellular Therapy will take place 4:20 – 5:50 p.m. MST in Ballroom AB of the Salt Palace Convention Center.
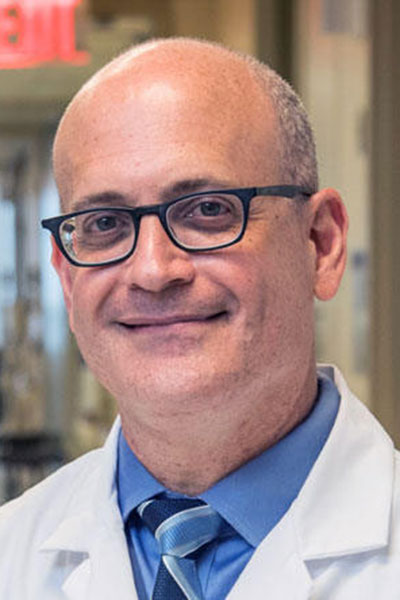
“This topic remains very urgent and of high priority,” said Ran Reshef, MD, MSc. “Relapse today is the No. 1 cause of death after transplant. We’ve made tremendous progress in the treatment of graft-versus-host disease (GVHD) and prevention of GVHD. We’ve also made tremendous progress in the management and prevention of infectious complications. We have not made significant progress in the prevention of relapse, and I think our field in general, for the next couple of decades, should be focused on trying to make sure that relapse risk is minimized as much as possible.”
As one of three featured speakers in the session, Dr. Reshef, professor of medicine and director of the cell therapy program at Columbia University Irving Medical Center, will review what he calls the “natural evolution” of merging transplantation and cellular therapies and engineered cell therapies with the goal of eliminating disease post-transplant.
“It has the potential of becoming a paradigm shift of how we will do transplants more efficiently in humans, more effectively and safer,” he said, pointing out that the oldest and one of the most potent forms of immunotherapy — allogeneic stem cell transplant — is an effective but blunt instrument. Replacing a patient’s entire bone marrow to induce graft-versus-leukemia response comes at the price of a high risk of GVHD. More precision engineering methods present a promising avenue to preventing relapse post-transplant.
Dr. Reshef said the new approach differs from current autologous CAR T therapy because it takes potent cancer-killing T-cells that have been identified as recognizing specific targets from the same donor who has already provided bone marrow transplant to the patient.
“These will basically be allogeneic CAR T-cells or allogeneic TCR cells, but they will not be rejected,” Dr. Reshef explained.
“Superimposing an engineered cell approach on transplant gives additional opportunities because we can actually leverage the mismatch between the donor and the recipient to create engineered donor cells that are going to be specific against only recipient cells,” Dr. Reshef continued. “So, they may not need to identify the leukemia; they just need to identify all recipient hematopoietic cells in general.”
Additionally, clinical trials have already shown that these strategies are significantly safer than a standard donor lymphocyte infusion, he said.
Dr. Reshef will be joined by Christopher Hourigan, DM, DPhil, FRCP, a professor and the director of the Virginia Tech Fralin Biomedical Research Institute Cancer Research Center, and Sun Loo, MBBS, FRACP, FRCPA, a clinical hematologist in Australia. Dr. Hourigan will discuss MRD in patients with AML before and after allogeneic HCT. Dr. Loo will address small molecule development in the context of HCT. Saar Gill, MD, PhD, professor of medicine at the University of Pennsylvania and director of the Translational Center of Excellence in Genetically Engineered Hematopoietic Cell Transplantation, will serve as the session’s chair.
Watch 2026 Tandem Meetings sessions on demand

If you aren’t able to make it to a live session during the 2026 Tandem Meetings — or you want to revisit a session — you can watch on-demand recordings within hours of the live presentations via digital access.
 Follow ASTCT®
Follow ASTCT®